
Comprehensive sexual and reproductive health (SRH) care requires a constellation of methods and services to help ensure individuals have safe and satisfying sex lives free of disease or infirmity, are able to have children if, when, and how often they want, and can safely navigate pregnancy and childbirth. Yet, at some point in their lives, a majority of people of reproductive age will lack access to adequate SRH services or become dissatisfied with the currently available methods. This large unmet need for SRH – with wide-reaching impacts on an individuals' health and broader family well-being – calls for continued innovation beyond existing methods and services to better meet the needs of diverse individuals over the course of their lives.
Despite the need for innovation and the clear link between SRH and achievement of global Sustainable Development Goals, funding for contraceptive research and development (R&D) has stagnated since 2018 (totaling USD 117 million in 2021). Similarly, funding for multipurpose prevention technologies that could address more than one SRH concern has also stagnated since 2018 (totaling USD 50 million in 2021). Working within these restrictive R&D resources, we need to put user perspectives and preferences as a top priority during the development process.
In research and development, product developers are trained to focus on finding "silver bullet," cure-all technologies for health problems. On rare occasions, one technology can do the trick (the polio vaccine, for example), but for the most part, one medication or technology cannot meet all user's needs. The SRH methods we develop, regardless of efficacy, can only be impactful if people actually want to use them. Over the last 70 years at the Population Council, we have always found individuals throughout their reproductive life cycles want an array of options. Our early investments in developing long-acting reversible contraceptive methods (such as intrauterine devices and implants) were born of this unmet need. As efficacious and safe as these long-acting methods are, their benefits are sometimes, outweighed by hesitancy and misgivings around provider-dependent long-acting methods. Looking to the broad social and demographic trends shaping our world – such as, shifting household structures, deepening inequities in health outcomes, increasing mobility and displacement, overburdened and understaffed health systems, persistent gender equality – a new array of SRH products are needed to meet individuals where they are and reduce the burden on health care providers and health systems.
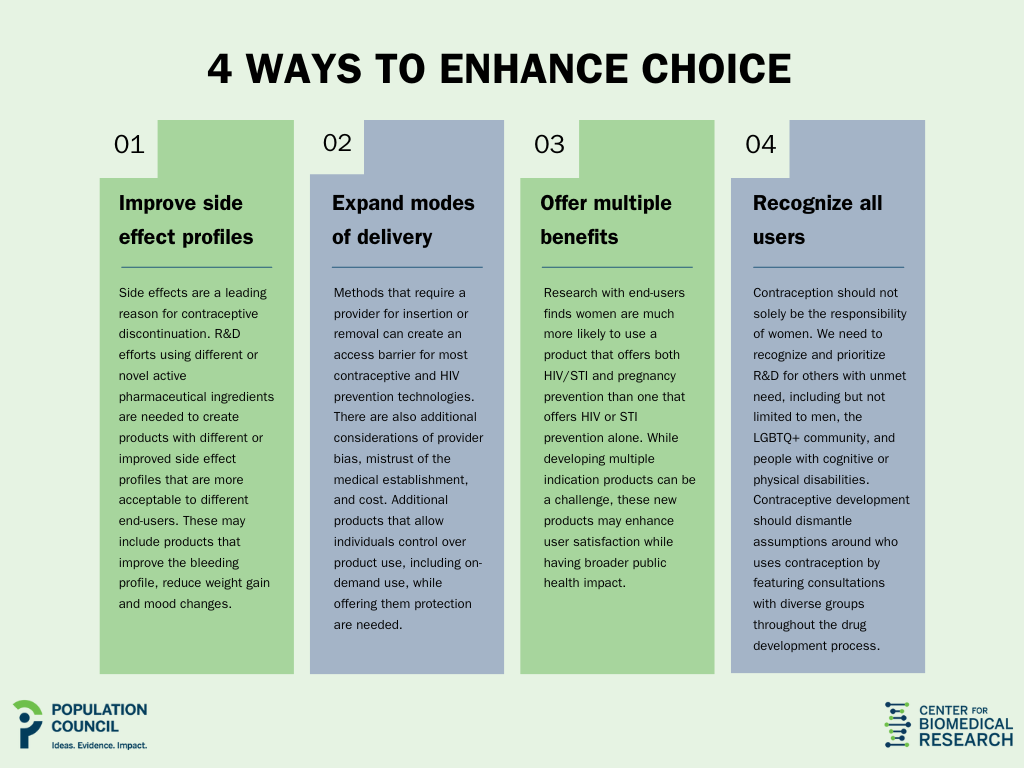
To achieve this, a renewed focus is needed for SRH product R&D. We propose prioritization of products that can:
(1) Improve side effect profiles. Side effects are a leading reason for contraceptive discontinuation. R&D efforts using different or novel active pharmaceutical ingredients are needed to create products with different or improved side effect profiles that are more acceptable to different end-users. These may include products that improve the bleeding profile, reduce weight gain and mood changes.
(2) Expand modes of delivery. Methods that require a provider for insertion or removal can create an access barrier for most contraceptive and HIV prevention technologies. There are also additional considerations of provider bias, mistrust of the medical establishment, and cost. Additional products that allow individuals control over product use, including on-demand use, while offering them protection are needed.
(3) Offer multiple benefits. Research with end-users finds women are much more likely to use a product that offers both HIV/STI and pregnancy prevention than one that offers HIV or STI prevention alone. While developing multiple indication products can be a challenge, these new products may enhance user satisfaction while having broader public health impact.
(4) Recognize all users. Contraception should not solely be the responsibility of women. We need to recognize and prioritize R&D for others with unmet need, including but not limited to men, gender diverse populations, and people with cognitive or physical disabilities. Contraceptive development should dismantle assumptions around who uses contraception by featuring consultations with diverse groups throughout the drug development process.
On World Contraception Day, the importance of choice in the realm of SRH cannot be overstated. Reproductive choice, made accessible without provider bias and accompanied by comprehensive sexual education and counselling, empowers individuals to make informed decisions that align with their reproductive values and goals. We cannot achieve these goals without an expanded array of options and sufficient investment. R&D funding must react to these steps so products may provide people with the ability to exercise choice and control over their reproductive lives, whether that means preventing unintended pregnancies, managing their sexual health, or achieving pleasurable and satisfying sexual lives.
